Autologous Transplants: A Beacon of Hope in the Fight Against Neuroblastoma
Neuroblastoma is a word that strikes fear into the hearts of many parents. It's a complex and aggressive cancer, primarily affecting children, that can leave families feeling desperate for effective treatment options. But what if there was a beacon of hope in the form of a cutting-edge medical procedure?
Enter autologous transplant, a treatment that's making waves in the fight against neuroblastoma. But what exactly is an autologous transplant, and how does it work? Is it truly a game-changer in pediatric oncology?
Let’s explore these questions and the intricacies of this promising therapy.
Understanding Neuroblastoma: The Enemy in Focus
- Neuroblastoma originates in the nerve tissues of infants and young children, most commonly in the adrenal glands.
- Unlike other cancers, neuroblastoma can spread rapidly to other parts of the body, making early detection and aggressive treatment crucial.
- Traditional treatments include surgery, chemotherapy, radiation therapy, and stem cell transplants.
- However, the survival rates vary significantly based on the stage at diagnosis and the patient’s response to treatment.
What is an Autologous Transplant?
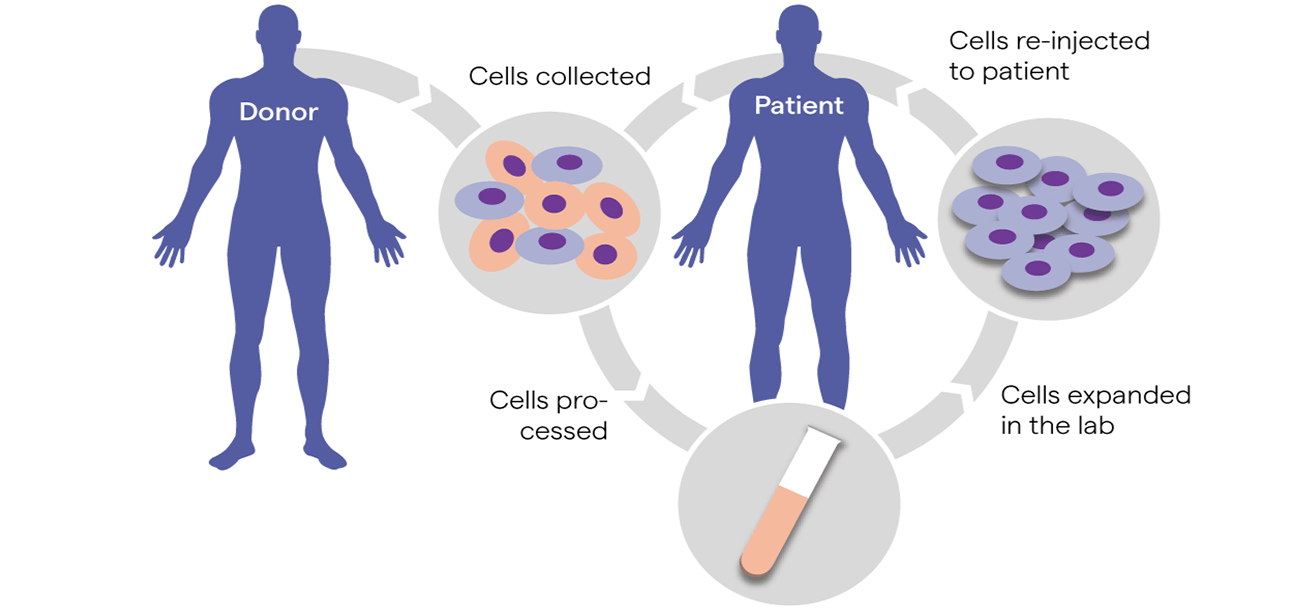
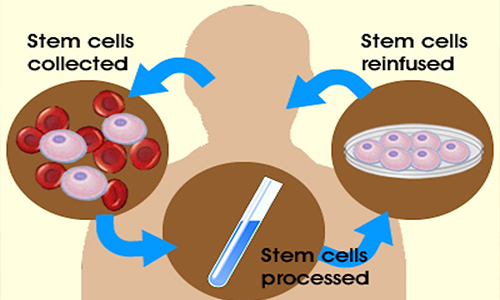
- Autologous transplant, also known as autologous stem cell transplant, involves harvesting a patient's own stem cells, which are then used to replace damaged or destroyed bone marrow.
- This procedure is particularly beneficial after high-dose chemotherapy, which, while effective at killing cancer cells, also destroys healthy bone marrow cells.
- By using the patient's own cells, the risk of rejection and complications associated with donor cells is minimized.
The Process of Autologous Transplant: Step by Step
Stem Cell Collection
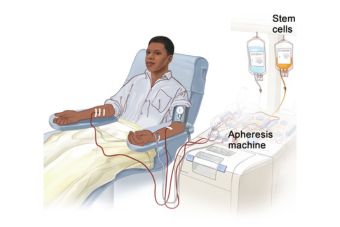
The first step involves collecting stem cells from the patient's blood or bone marrow. This is usually done after initial rounds of chemotherapy when the number of healthy stem cells is at its peak.
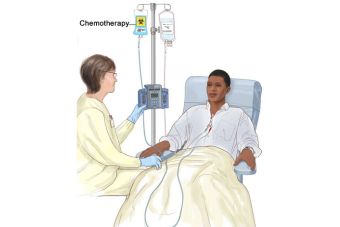
High-Dose Chemotherapy
The patient undergoes high-dose chemotherapy to eradicate as many cancer cells as possible. This phase is critical and aims to maximize the treatment’s effectiveness.
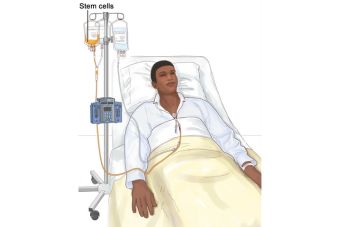
Stem Cell Infusion
After chemotherapy, the collected stem cells are infused back into the patient's bloodstream. These cells migrate to the bone marrow, where they begin to produce new, healthy blood cells.
Recovery
The recovery period involves close monitoring as the new bone marrow cells take root and begin to function. Patients are at a high risk of infections during this time, so supportive care is essential.
Benefits of Autologous Transplant in Neuroblastoma
Autologous transplants offer several benefits in treating neuroblastoma
- Reduced Risk of Rejection: Since the stem cells come from the patient, the body is less likely to reject them, leading to a smoother recovery process.
- High-Dose Chemotherapy: Allows for more aggressive treatment of cancer, which can be particularly important in high-risk neuroblastoma cases.
- Improved Survival Rates: Clinical studies have shown that autologous transplants can improve survival rates in children with high-risk neuroblastoma, offering a better prognosis for many patients.
Challenges and Considerations
While promising, autologous transplants are not without their challenges

Intensive Process
The procedure is complex and requires a significant time commitment from both the medical team and the family.

Potential Complications
Risks include infection, bleeding, and other complications related to high-dose chemotherapy and the transplant process.

Cost and Accessibility
The procedure can be expensive and may not be readily available in all medical centers, posing a barrier for some families.
Real-Life Success Stories: Testimonials from the Frontlines
Consider the story of Emma, a six-year-old diagnosed with stage IV neuroblastoma. After conventional treatments failed to halt the progression of her cancer, her medical team recommended an autologous transplant. The process was arduous, but today, Emma is in remission, attending school, and living a normal life. Her parents attribute her recovery to the aggressive treatment made possible by the autologous transplant. Stories like Emma’s highlight the potential life-saving impact of this treatment.
The Future of Autologous Transplants in Neuroblastoma
- Research is ongoing to enhance the effectiveness of autologous transplants.
- Innovations such as combining transplants with novel therapies like immunotherapy and targeted treatments are showing promise.
- The goal is to not only increase survival rates but also improve the quality of life for survivors.
Conclusion: A Beacon of Hope
- Autologous transplant represents a beacon of hope for children battling high-risk neuroblastoma. While the journey is challenging, the potential benefits make it a viable and often life-saving option. As research continues to advance, this treatment could become even more effective, offering new hope to families facing the daunting diagnosis of neuroblastoma.
- Is autologous transplant the definitive answer to neuroblastoma? Only time and ongoing research will tell. However, it stands as a powerful tool in the fight against this aggressive cancer, offering renewed hope and brighter futures for many young patients. Dr. Shweta Bansal, consultant Pediatric Hemato-Oncology in Mumbai, emphasizes the importance of such treatments in transforming patient outcomes.
- For parents navigating the complexities of neuroblastoma treatment, exploring the option of an autologous transplant with their healthcare team, including experts like Dr. Shweta Bansal, consultant Pediatric Hemato-Oncology in Mumbai, could be a crucial step towards achieving remission and recovery for their child.
- If you or a loved one is facing a neuroblastoma diagnosis, consider consulting with specialists who can offer advanced treatments like autologous transplants. Renowned specialists, including Dr. Shweta Bansal, consultant Pediatric Hemato-Oncology in Mumbai, are available to guide you through this challenging journey. Schedule a consultation today to explore all available treatment options and take the first step towards a brighter, cancer-free future.
Copyright © Childhood Cancer Care | Dr. Shweta Bansal.